Factors such as age, health, sex and species affect the outlook after death. This case is seen in the challenge of culture and transplantation of metabolically active islet cells from donor to recipient. Researchers believe that autoimmune processes, high energy costs and destruction of protective mechanisms can be the cause of many islet cell transplant failures.
How the interplay of these variables allows certain cells to continue functioning after the death of the organism is not clear. One of the hypotheses proposed in this field is that the special channels and pumps embedded in the outer membrane of cells act as complex electrical circuits. These channels and pumps generate electrical signals that allow cells to communicate with each other and perform specific functions such as growth and movement, and affect the specific structure of the organism.
The rate of change of cell types after death is also unclear. Past research has shown that certain genes involved in stress, immunity, and epigenetic regulation are active after death in mice, zebrafish, and humans, and this indicates a broad potential for transformation among cell types.
Biological and medical implications
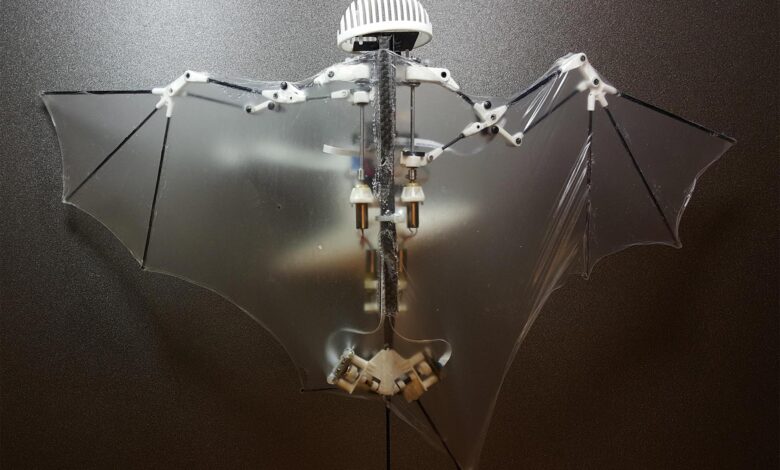
The third mode not only provides new insights into the adaptation of cells but also offers prospects for new therapies. For example, enterobots can be made from living human tissue to deliver drugs without triggering an unwanted immune response. Engineered enterobots injected into the body may be able to clear arterial plaque in people with atherosclerosis and remove excess mucus in patients with cystic fibrosis.
The important thing is that these multicellular organisms have a limited life span and after four to six weeks they naturally degrade. This “death key” prevents the growth of potentially invasive cells.
A better understanding of how some cells continue to function and transform into multicellular entities after an organism dies holds promise for personalized and preventive medicine.